Hiatal hernias are unique in that they sometimes produce little or no noticeable symptoms and surgery isn't always needed.
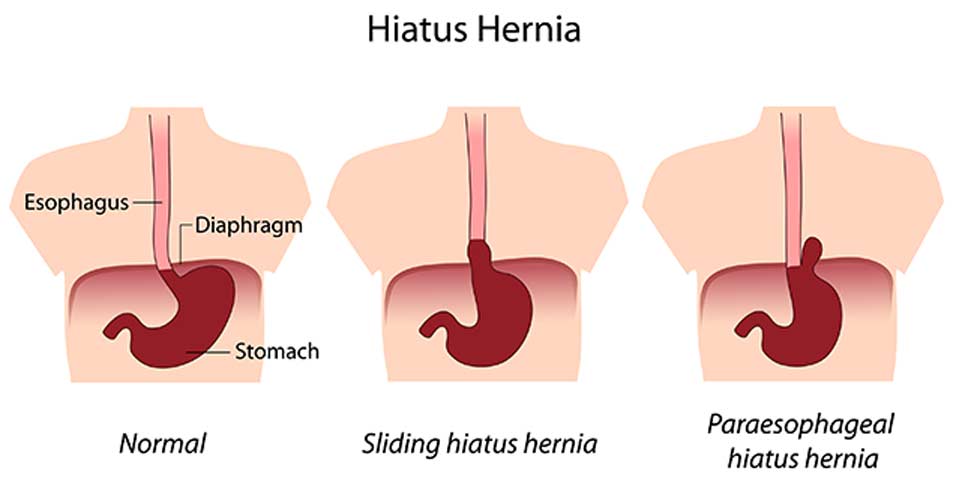
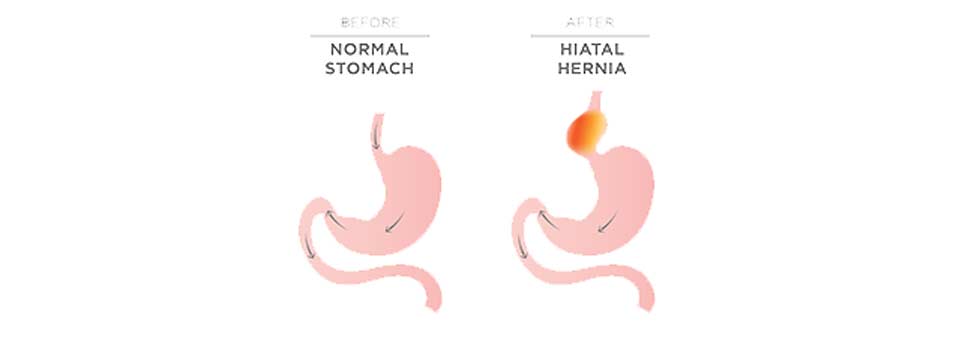
Sometimes accompanied by abdominal pain or heartburn, a hiatal hernia refers to a protrusion of a portion of the upper stomach through a weak spot in the diaphragm muscle that separates the abdomen and chest.
It’s entirely possible to have this type of hernia and not know it until testing is done for another unrelated condition.
CONTACT US TODAY
How Might a Hiatal Hernia Develop?
Like any hernia, a hiatal hernia tends to develop because muscle tissues are weak or thin. In this case, it’s the area where the stomach links to the diaphragm that’s affected. Possible reasons for the development of a hiatal hernia include age-related changes with tissues and structures in the upper abdominal area, some types of surgery, certain injuries, sudden trauma, and consistent pressure on muscles in the upper abdominal region from things like heavy lifting, difficult bowel movements, or chronic coughing. Some individuals are also born with an excessively large esophageal hiatus that could increase the risk of developing a hiatal hernia.
What Are Possible Hiatal Hernia Symptoms?
Smaller or minor hiatal hernias are the ones that normally produce no symptoms. It’s usually mid-size or larger hernias of this nature that tend to have more disruptive or noticeable symptoms associated with them. Some hiatal hernia sufferers may mistakenly assume they have acid reflux of heartburn if their primary symptoms include a back-up of stomach acid into the esophagus or food or beverages returning to the mouth. Additional symptoms related to a hiatal hernia may include:
- Shortness of breath
- Difficulty swallowing
- Pain in the chest or abdominal area
- Passing dark stools or vomiting blood – possible sign of related gastrointestinal bleeding
How Is a Hiatal Hernia Diagnosed?
Because of the heartburn symptoms often associated with hiatal hernias, diagnosis is often made when tests are done to find out why persistent heartburn symptoms are being experienced. Upper digestive system X-rays are done after consuming a chalky liquid that coats to the digestive tract to improve the clarity of images, an upper endoscopy done with a flexible, lighted tube attached to a lens, and an esophageal manometry to measure rhythmic muscle contractions while swallowing are among the common tests performed that often lead to a hiatal hernia diagnosis.
What Are Available Treatment Options?
If there are no disruptive symptoms, treatment for a hiatal hernia is typically not necessary. Otherwise, medications are usually recommended to manage heartburn/acid reflux symptoms. If medication isn’t effective, surgery may be done to remove the hernia sac and return tissues and structures to their original position. Some patients need to have their esophageal sphincter reconstructed as well. With laparoscopic surgery, smaller incisions, a tiny camera, and special tools are used to make the procedure less invasive.
The risk of developing a hiatal hernia is greater for individuals who are overweight and those 50 and over. Symptoms of an existing hernia in the diaphragm area can be aggravated by any type of pressure on the stomach. Odds of experiencing further complications may also be minimized by eating a healthy diet that includes foods that are easy to digest, avoiding overly acidic foods, and getting regular exercise to help keep weight in check and strengthen muscles around the stomach and diaphragm.

